Which of the following is the most appropriate next step in management for this patient’s condition?
- A) IV Physostigmine
- B) IV Potassium iodide
- C) IV Propranolol
- D) PO Propylthiouracil (PTU)
This patient presents to the Emergency Department with altered mental status. This presenting symptom can be due to a large variety of etiologies, including hypoglycemia, sepsis, toxic ingestions, electrolyte abnormalities, stroke, and more. The management and evaluation of a patient with altered mental status depends on the primary assessment of the patient (“ABCs”, or Airway, Breathing, Circulation) to identify any acute life-threatening conditions that need to be managed emergently, the history, and the physical examination. One mnemonic that may help in remembering the many causes of altered mental status is “AEIOUTIPS”. The table below outlines this mnemonic.

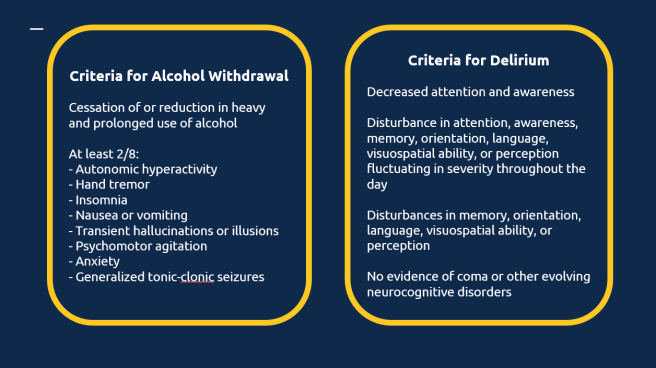
This patient arrives hyperthermic, tachycardic in atrial fibrillation, diaphoretic, and altered with psychotic behavior. Thyroid storm, the most severe manifestation of hyperthyroidism, should always be on the differential diagnosis in patients with fever and altered mental status. Other considerations are sepsis, sympathomimetic overdose, anticholinergic overdose, serotonin syndrome, and pheochromocytoma.
This patient has thyroid storm, a life-threatening endocrine emergency that requires prompt recognition and treatment. Symptoms of thyroid storm include altered mental status, psychosis, seizures, coma, tachycardia, atrial fibrillation, high-output heart failure, dyspnea, vomiting, diarrhea, weight loss, and anterior neck enlargement. Severe hyperthyroidism should have a low-undetectable TSH level with elevated T3/T4 levels, but in acute illness these levels may be unreliable. For this reason, the diagnosis and treatment of thyroid storm should be based on clinical grounds.
An anticholinergic toxidrome can appear similar to this patient with tachycardia, hypertension, agitation, and altered mental status. A key differentiating factor is diaphoresis. Patients with anticholinergic ingestions should have dry skin, not wet skin. The treatment for anticholinergic toxicity is benzodiazepines and IV physostigmine (Choice A) if symptoms are unresponsive to benzodiazepines. Physostigmine is not the best next step in this scenario.
Treatment of thyroid storm is algorithmic. First, beta blockade (Choice C) should be given to control the heart rate and block T4 to T3 conversion, next anti-thyroid medications (Methimazole or Propylthiouracil (Choice D)) should be given to block thyroid hormone synthesis, and lastly corticosteroids and inorganic iodine (Choice B) can be given to block release of stored thyroid hormone. The best next step in managing this patient with thyroid storm is administration of IV Propranolol (Choice C). Propranolol helps manage the tachycardia, systemic symptoms, and also inhibits conversion of T4 to T3.
Correct Answer: C
References
- Alvarez, A & Sekhon, N. (2019). Altered Mental Status. Society of Academic Emergency Medicine. Retrieved from https://www.saem.org/cdem/education/online-education/m4-curriculum/group-m4-approach-to/approach-to-altered-mental-status
- Lee, T. (2013). Diagnosing hyperthyroidism: Answers to 7 common questions. ALiEM. Retrieved from https://www.aliem.com/diagnosing-hyperthyroidism/
- Swaminathan, A. (2017). Thyroid Storm. CORE-EM. Retrieved from https://coreem.net/core/thyroid-storm/
Sharing is caring
- Click to share on Twitter (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to email a link to a friend (Opens in new window)
- Click to print (Opens in new window)